
Nutrition and Hydration Week 2025
Nutrition and hydration week is a social movement which supports positive discussions between healthcare professionals and patients to help people struggling to maintain good levels of nutrition. This information is important, however, for both patient and clinician; for the clinician to offer the best guidance, and for the patient to know which questions to ask. This article will aim to offer a balanced perspective to aid the process.
The importance of good nutrition and hydration
There’s an ancient saying about food and the power of healing: “Let food be thy medicine and medicine be thy food”. This has been hotly contested as food is strictly not medicine nor vice versa, so is not to be taken literally. But what we know is that a carefully balanced diet with all nutrients needed to sustain a healthy body will be better able to cope with life’s challenges.
If your body is already ‘challenged’ with a bladder and bowel condition, diet can become a little more tricky. What if you can’t eat what’s deemed healthy because it aggravates your symptoms? Or if you struggle with key food groups because they cause you issues? You may have severe allergies or intolerances which affect how you choose and prepare food. If you find achieving a balanced diet and fluid intake more difficult with a bladder or bowel condition, you’re not alone.
According to research, there are around 3 million people at risk of malnutrition in the UK, 1.3m of which are over 65 years of age. Meanwhile a staggering 10% of children are living with food insecurity. The reasons for malnutrition are believed to vary; they likely include low income households, people who struggle to prepare meals due to a disability or illness, or those who have an existing health condition. There will be other contributing factors or perhaps a combination of reasons people struggle to achieve the ideal balanced diet.
What is food insecurity?
Food insecurity is where a person doesn’t have reliable access to nutritious food, which means they may not be able to follow a regular meal routine.
What is malnutrition?
This is defined as an imbalance of nutrients in the body, which prevents it from functioning properly. It includes over-nutrition (too many nutrients for the body to use) or under-nutrition (not enough nutrients).
What are nutrients, and how do you know if you’re getting enough?
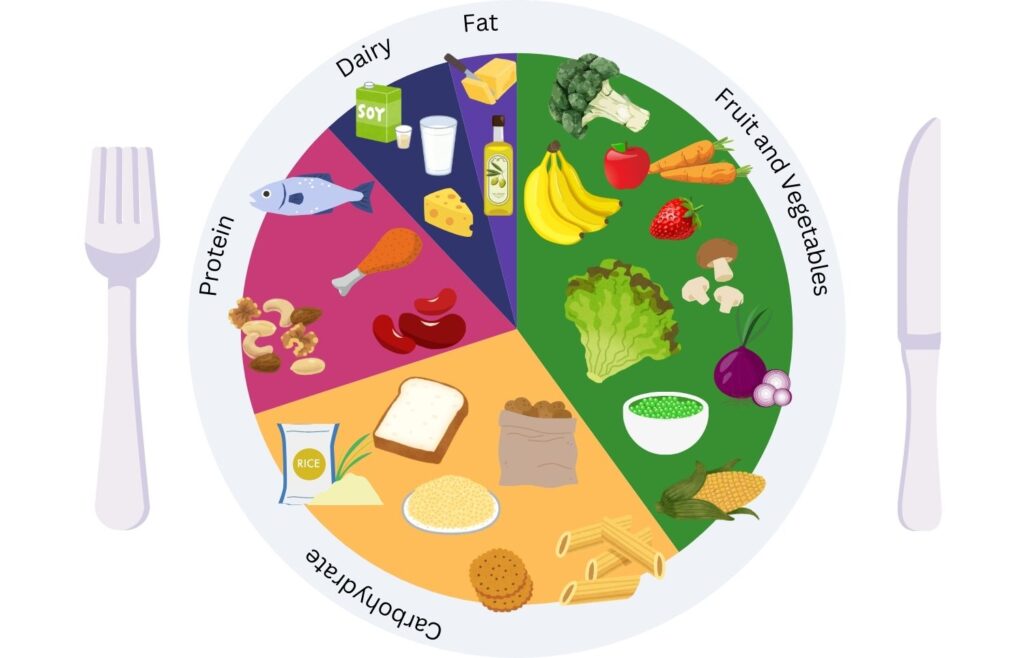
There are 6 main nutrient groups which include proteins, carbohydrates, fats, vitamins, minerals, and fluids. Our bodies need all of these things in various proportions and frequencies in order to function optimally. You can learn more about what foods belong to below.
- Carbohydrates are needed for energy – found in bread, pasta, rice, fruit, and sugar
- Proteins support growth and repair – found in meat, beans and pulses, nuts, eggs and seafood
- Fats are important for storing energy – saturated fats come from dairy products and meat, and the healthier unsaturated fats from avocado, oily fish, olives and nuts.
- Vitamins support all of the functions of the body, and a good balance is important for maintaining healthy skin, bones, eyesight, immune system function and repairing. Look out for fruits and vitamins high in Vitamins A, B, C, D and K.
- Minerals similarly support the immune system and metabolism, oxygen supply, kidney function and good bone health. Look out for foods that contain magnesium, calcium, zinc, iron, potassium and sodium. Potassium and phosphorus are also key to organ and bone health respectively.
- Lastly but no less important, is Water.
What does a balanced meal look like?
The below pictogram shows an example of amounts of each food group for your plate – keep fats to a minimum, and drink water at every meal time as well as in between.
Your diet should contain a high proportion of greens, vegetables and fruit – around a third or more your daily intake. A variety of ‘rainbow vegetables’ offer a wide range or vitamins and minerals essential for your immune system and daily function. Many fruits also contain both soluble fibre (in the fruit flesh) and insoluble fibre (in the skin) to aid digestion.
Carbohydrates found in pasta, potatoes and bread support energy levels – choose wholewheat varieties wherever possible which offer slower energy release and provide you with more vitamins and minerals than white alternatives. If you can, prepare potatoes with their skins on, to provide more fibre – the flesh of the potato however, still contains ample vitamins and nutrients. Sugar is also a carbohydrate, providing energy for the body in the quickest form.
Proteins are vital for your body, acting as the building block for tissues, muscles and organs while also supporting immune function, aiding in energy production and helping with fluid and pH balance. This ‘build’ function makes protein essential when recovering from surgery, to aid tissue repair and prevent infection.
Dairy (or fortified soya/alternatives) are rich in calcium which aids strong bone growth in children, and maintaining bone density as we age. Dairy products are also high in potassium which helps moderate blood pressure. Keep dairy intake a little lower, as it tends to be higher in fat, or choose 1% varieties.
When it comes to oils and fats, keep these under control – Our bodies do need some fat, as it helps us to absorb vitamins A, D and E. Try to include more unsaturated fats in your diet such as avocado, nuts, olive oil, than saturated fats such as from meat, cheese and palm oil.
Be cautious if you take vitamin supplements, as the amounts your body can store and use may vary. This is general guidance for a balanced diet, as per NHS guidelines. There are a plethora of choices when it comes to food – both what you eat and how you eat it – which you may wish to explore further. These include the effects of intermittent fasting, FodMap diets, plant-based foods for sustainability, and focussing on whole foods, but if you’re making drastic changes it’s worth seeking advice to ensure this will meet your particular needs.
If you need advice, please visit your healthcare practitioner or consult a registered Dietitian. Find out more about portion sizes in the NHS Eatwell guide.
Find out more about portion sizes in the NHS Eatwell guide.
Nutrition for a bladder or bowel condition
Certain conditions can affect what you eat or drink, due to causing flareups in symptoms. The most common of these include IBS, Diverticular Disease and people who live with a stoma.
Diverticular Disease
If you live with Diverticular Disease, or regularly experience Diverticulitis, it’s important to eat a healthy balanced diet which includes plenty of whole grains, fruit and vegetables, and drink plenty of water to aid digestion.
Stoma Diet
Ostomates may need to avoid or limit certain foods which can cause issues. Some people may be advised to avoid eating very fibrous foods or foods with tough outer skins such as sweetcorn, peas, popcorn and potato skins to avoid causing a blockage in the bowel. It’s also advisable to avoid fizzy drinks if you tend to produce a lot of gas. For more, read our article on diet and exercise with a stoma.
Diet for IBS
People with IBS may wish to avoid onions, garlic, cauliflower, beans and pulses which set off your symptoms. Instead, aim for vegetables such as cabbage carrot, courgette, cucumber, lettuce, olives, parsnips, peppers, plantain potato, pumpkin, spinach, rocket, tomatoes, radish, rocket, spinach, water chestnuts or yam. Remember, not everyone’s sensitive gut is the same, as lots of other lifestyle factors and foods have an effect on how our gut functions. So you may wish to try small amounts of foods to determine what works for you. Find out more about IBS and food.
Some general advice to help aid digestion includes:
- Follow a healthy, balanced diet
- Minimise or manage stress – there are some great apps available to help with mindful walking, improving sleep etc
- Stay active. A gentle walk or swim will help alleviate stress and help control your symptoms.
Hydration with a Bladder or Bowel Condition
It is important to drink enough fluid such as water each day to keep the bladder healthy, otherwise the bladder will not work as it should. If you don’t drink enough, the bladder gets used to holding smaller amounts of urine and can become sensitive. This is especially the case if your urine becomes more concentrated, as it is more likely to irritate your bladder.
Similarly, fluid intake is important to aid digestion. If you don’t drink enough water, the stool in the bowel can become difficult to pass. You can also become more prone to certain conditions, including:
- Constipation
- Headaches
- Urinary tract infections (UTIs)
- Kidney stones
Caffeine can irritate the bladder so try to avoid tea, coffee and caffeinated soft drinks such as cola or energy drinks. Acidic fruit juice can also irritate the bladder, as well as hot chocolate. Instead, opt for herbal teas or decaffeinated tea and coffee.
Our advice is always to choose water first, and carry a refillable bottle so you can sip throughout the day.
Nutrition and Hydration Week Principles
Nutrition & Hydration Week keenly promotes the following principles to support clinicians and patients manage diet, including:
The 10 Key Characteristics for Good Nutritional Care
This is a list of principles that all healthcare practitioners should carry out to ensure good nutritional information and care is delivered to all patients.
Protected Mealtimes – Ensuring patients can eat uninterrupted in hospitals – this is a principal that we can all adopt at home, with no screens at mealtime for example, or making the time to sit at a table and share a meal with others whenever possible.
Highlighting Good Nutrition and Hydration Practices
Nutrition advocates, often dietitiens could advise on diet to promote healthy outcomes or help prevent disease, and minimum standards for all settings around nutritional information.
Continued Education for professionals on good nutrition and hydration – Including events such as the Global Tea Party on the Wednesday of Nutrition and Hydration Week to help share resources and come together to talk about nutrition.
Nutrition and Hydration week is aimed at highlighting the actions that clinicians should be taking in order to adequately inform patients about nutrition and hydration, to help individuals become empowered to manage their own nutritional needs. As a patient led organisation, we feel its important for patients to understand what works for you (as this could differ greatly from others you know, even if they have the same condition) and implement small changes towards drinking plenty of fluid, and maintaining a healthy nutritious diet.
Useful Resources
We’ve pulled together some key resources you may wish to share, from the bladder and bowel hub as well as other sources.
Nutrition and Hydration Week Resources – for Healthcare Professionals
Guide to Healthy Nutrition and Hydration in Older Age – This guide considers risks in adult healthcare, as well as adjusting diet as we get older.
NHS BMI Calculator – Find out what your body composition is, and what you could do to improve your diet.
Fluid Matrix – how much should you be drinking for your size? Find out with this chart.
Healthy Drinking – a guide to which drinks irritate the bladder





